Magnesium Glycinate: A Comprehensive Clinical and Mechanistic Review
The Essential Role of Magnesium in Human Physiology
Magnesium as a Fundamental Biological Cofactor
Magnesium (Mg2+) is an essential mineral and the second most abundant intracellular cation in the human body, surpassed only by potassium.1 Its biological importance cannot be overstated; it functions as a critical cofactor—a helper molecule—in more than 600 enzymatic reactions that sustain health and life.1 Every cell in the body contains magnesium and requires it to function, underscoring its foundational role in human physiology.2 An average adult body contains approximately 25 grams of magnesium, with 50-60% of this reserve stored within the skeletal system, highlighting its structural importance.2
The vast biochemical network dependent on magnesium includes several core life-sustaining processes:
-
Energy Creation: Magnesium is indispensable for energy metabolism, particularly in the synthesis and stabilization of adenosine triphosphate (ATP), the body's primary energy currency. It acts as a cofactor in the enzymatic reactions that convert food into usable energy.2
-
Protein Synthesis: It is fundamentally involved in the creation of new proteins from amino acids, a process essential for growth, repair, and maintenance of all body tissues.2
-
Genetic Maintenance: Magnesium plays a key role in the synthesis, repair, and stability of DNA and RNA, the building blocks of life.2
-
Neuromuscular Function: The mineral is vital for maintaining normal nerve transmission and muscle function. It is integral to the process of muscle contraction and, crucially, muscle relaxation.4
-
Cardiovascular Regulation: Magnesium contributes to keeping the heartbeat steady and helps regulate blood pressure, supporting overall cardiovascular health.3
-
Skeletal Health: While calcium receives much of the attention, magnesium is also essential for strong bones. It contributes directly to bone crystal formation and indirectly by helping to regulate the levels of calcium and vitamin D, two other nutrients vital for bone health.3
-
Immune System Support: It plays a supportive role in maintaining a healthy and responsive immune system.4
Homeostasis, Deficiency, and a Modern Health Concern
The body maintains magnesium balance, or homeostasis, through a tightly regulated system involving intestinal absorption and renal excretion. Specialized ion channels in the intestine, such as the Transient Receptor Potential Melastatin type 6 and 7 (TRPM6 and TRPM7), play a key role in its uptake from the diet, while the kidneys precisely control how much is retained or excreted in the urine.1
Despite these regulatory systems, magnesium deficiency is a significant and often overlooked health concern. Hypomagnesemia is clinically defined as a serum magnesium level below 1.8 mg/dL.6 Early symptoms of deficiency can be vague and include loss of appetite, nausea, vomiting, fatigue, and weakness.4 As the deficiency becomes more severe, symptoms can escalate to include numbness, tingling, muscle contractions and cramps, seizures, personality changes, and abnormal heart rhythms. Severe deficiency can lead to secondary electrolyte imbalances, including low blood calcium (hypocalcemia) and low blood potassium (hypokalemia), because magnesium is required for their proper transport and metabolism.4
Several populations are at an elevated risk for developing magnesium deficiency. These include older adults, individuals with type 2 diabetes, those with alcohol use disorder, and people with gastrointestinal diseases that cause malabsorption, such as Crohn's disease or celiac disease.4 Furthermore, the use of certain common medications, including diuretics and proton pump inhibitors, can lead to magnesium depletion over time.1 Compounding these risk factors, dietary surveys consistently show that a substantial portion of the population in Western countries, with some studies suggesting up to 50-70% of adults, consumes less than the recommended daily amount of magnesium.2
A critical challenge in identifying magnesium deficiency lies in the limitations of standard diagnostic testing. Serum magnesium tests, the most common method of assessment, measure the concentration of magnesium in the blood. However, blood contains less than 1% of the body's total magnesium stores.10 The body works diligently to maintain stable serum magnesium levels, often at the expense of tissue stores, by pulling the mineral from bone and muscle when intake is low.7 Consequently, a normal serum magnesium level can mask a significant underlying intracellular or total-body deficiency. This paradox means a patient may present with classic symptoms of deficiency, such as muscle weakness or hyperexcitability, yet have a "normal" blood test result, potentially delaying or preventing appropriate intervention. This diagnostic gap underscores the importance of a more holistic clinical approach that considers dietary habits, lifestyle risk factors, and patient-reported symptoms, rather than relying solely on serum measurements. More advanced testing, such as red blood cell magnesium analysis, may provide a more accurate picture of the body's magnesium status but is not yet standard practice.11
The Landscape of Magnesium Supplementation: A Comparative Analysis
Understanding Bioavailability: Organic vs. Inorganic Salts
Given the prevalence of insufficient dietary intake, magnesium supplementation has become a common strategy for restoring adequate levels. However, not all magnesium supplements are created equal. Their effectiveness is largely determined by their bioavailability—the degree and rate at which the magnesium is absorbed by the body and becomes available for use.13
Magnesium supplements can be broadly categorized into two main groups: inorganic salts and organic compounds. Inorganic salts, such as magnesium oxide and magnesium chloride, involve magnesium bound to an inorganic element. Organic compounds involve magnesium bound to an organic acid (e.g., citric acid) or an amino acid (e.g., glycine). A guiding principle in magnesium supplementation is that organic forms generally exhibit higher water solubility and, consequently, greater bioavailability than their inorganic counterparts.13
-
Magnesium Oxide (MgO): This form has a high percentage of elemental magnesium by weight, making it appear potent on a label. However, it is poorly absorbed by the body and is well-known for its strong osmotic laxative effect, making it a common ingredient in constipation remedies but a poor choice for correcting a systemic deficiency.14
-
Magnesium Citrate: This is an organic salt formed by combining magnesium with citric acid. It is considered to have high bioavailability, significantly better than magnesium oxide, and is effective for both repleting magnesium stores and providing gentle laxative action.14
-
Magnesium Malate: This organic form combines magnesium with malic acid, a compound involved in the body's energy production cycle. It is also highly bioavailable and has been studied for its potential role in conditions involving energy deficits, such as fibromyalgia.16
The Unique Chemistry of Magnesium Glycinate: The Power of Chelation
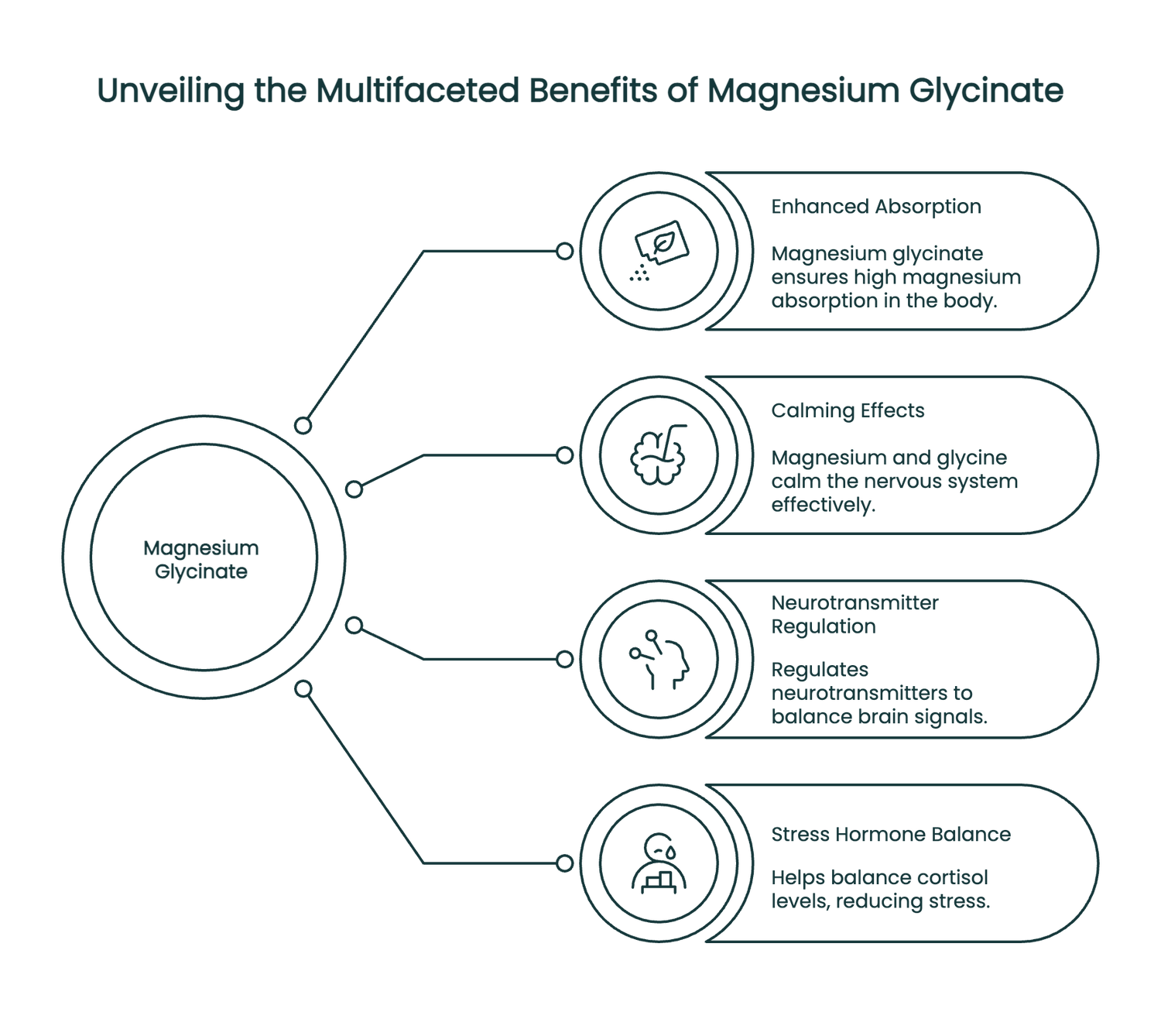
Among the various organic forms, magnesium glycinate (also known as magnesium bisglycinate) stands out due to its unique chemical structure and superior properties. It is a chelated form of magnesium, created by a process where one magnesium ion is bonded to two molecules of the amino acid glycine.15 This chelation process forms highly stable, five-membered ring structures that electrically neutralize the magnesium ion.15
This stable, neutral structure confers several distinct advantages. First, it protects the magnesium ion from binding with dietary inhibitors (like phytates) in the gut. Second, and most importantly, it allows for a different absorption pathway. While most mineral salts dissociate into ions that must compete for limited absorption channels in the intestine, magnesium glycinate can be absorbed in part as an intact dipeptide (magnesium bound to glycine).15 This absorption occurs via dedicated amino acid transporters in the proximal small intestine, which are more efficient and less saturated than ion channels. This unique absorption mechanism is a primary reason for its exceptionally high bioavailability.15
The most significant clinical benefit derived from this structure is its outstanding gastrointestinal (GI) tolerance. Because it is absorbed so efficiently and does not have the strong osmotic effect of unabsorbed salts, magnesium glycinate is remarkably gentle on the stomach.13 It does not typically cause the diarrhea or abdominal cramping associated with other forms like oxide or even citrate at higher doses.15 This makes it an ideal choice for individuals with sensitive digestive systems, those who require higher therapeutic doses, or anyone needing long-term supplementation without disruptive side effects.
It is also important for consumers to distinguish between "pure" and "buffered" magnesium glycinate. Pure chelate forms contain only magnesium bound to glycine. Buffered forms are mixed with a cheaper, less bioavailable form like magnesium oxide to increase the total elemental magnesium content per capsule.21 While this may seem appealing, it can compromise the very benefits—high bioavailability and GI tolerance—that make the pure chelate form desirable.
The Glycine Component: An Active Partner in Neuromodulation
The superiority of magnesium glycinate, particularly for neurological and psychological health, extends beyond its enhanced absorption. The glycine molecule itself is not merely an inert carrier; it is an active and important neurotransmitter in its own right.22 Glycine is recognized as the major inhibitory neurotransmitter in the brainstem and spinal cord.22
Glycine exerts its effects by binding to and activating glycine receptors, which are ligand-gated chloride (Cl−) channels on the surface of neurons.24 When activated, these channels open, allowing negatively charged chloride ions to flow into the neuron. This influx of negative charge hyperpolarizes the cell membrane, making the neuron less likely to fire an action potential. This inhibitory action is fundamental to calming the nervous system and is involved in processing motor and sensory information, as well as pain transmission.24
This makes magnesium glycinate a true dual-action compound. It delivers highly bioavailable magnesium, which itself has calming properties through its roles as a GABA agonist and NMDA receptor antagonist.26 Simultaneously, it delivers glycine, which provides its own direct inhibitory signaling in the central nervous system. This synergistic relationship, where two components with similar calming effects are delivered in a single, highly absorbable molecule, provides a powerful mechanistic rationale for its use in conditions characterized by nervous system hyperexcitability, such as anxiety, stress, and insomnia. This is a more profound advantage than simple GI tolerance and positions magnesium glycinate as a theoretically superior choice for targeting brain health.
The following table provides a comparative summary of the most common forms of magnesium supplements, facilitating an informed choice based on individual health needs and goals.
|
Table 1: Comparative Analysis of Common Magnesium Supplements |
|||||
|
Form |
Chemical Partner |
Relative Bioavailability |
Key Mechanisms/Properties |
Primary Clinical Uses |
Common Side Effects |
|
Magnesium Glycinate |
Glycine (amino acid) |
High |
Dual-action neuro-inhibitory (Mg + Glycine); chelated for stability; excellent GI tolerance. 15 |
Sleep, anxiety, stress, correcting deficiency, general supplementation. 16 |
Minimal; very gentle on the digestive system. 15 |
|
Magnesium Citrate |
Citric Acid |
High |
Highly soluble; acts as an osmotic laxative by drawing water into the intestines. 14 |
Correcting deficiency, constipation. 16 |
Diarrhea, abdominal cramping, especially at higher doses. 20 |
|
Magnesium Oxide |
Oxygen |
Low |
High elemental magnesium content but poorly absorbed; strong osmotic laxative effect. 14 |
Constipation, heartburn, indigestion. Not recommended for correcting deficiency. 16 |
Diarrhea, cramps; very likely to cause GI upset. 17 |
|
Magnesium Malate |
Malic Acid |
High |
Malic acid is a component of the Krebs cycle (energy production). Well absorbed. 16 |
Studied for fibromyalgia and chronic fatigue; correcting deficiency. 16 |
Generally well-tolerated with minimal GI side effects. 16 |
|
Magnesium L-Threonate |
Threonic Acid |
High (in brain) |
Specifically designed to cross the blood-brain barrier and increase magnesium levels in the brain. 18 |
Cognitive function, age-related memory issues, brain health. 16 |
Generally well-tolerated. |
|
Magnesium Sulfate |
Sulfur and Oxygen |
Variable |
Known as Epsom salt. Administered intravenously for clinical uses or used in baths. 18 |
IV use for eclampsia and seizures; used as a laxative. Bath use for muscle soreness. 18 |
GI upset when taken orally. Flushing with IV use. 5 |
Clinical Applications and Evidence: Neurological and Psychological Health
Sleep Regulation
Magnesium's role as a natural sleep aid is rooted in its profound effects on the central nervous system. Its reputation for promoting restful sleep is supported by several interconnected biochemical mechanisms.
Mechanisms
Magnesium's primary calming action stems from its ability to modulate key neurotransmitter systems. It acts as a natural antagonist of the N-methyl-D-aspartate (NMDA) receptor, a primary excitatory receptor in the brain.26 By partially blocking this receptor, magnesium reduces neuronal excitability, preventing the "racing thoughts" that can interfere with sleep. Simultaneously, it functions as an agonist, or promoter, of the gamma-aminobutyric acid (GABA) system, the brain's main inhibitory neurotransmitter.26 Magnesium is a necessary cofactor for the production of GABA, and by enhancing GABAergic activity, it promotes relaxation and helps initiate sleep.19
Beyond neurotransmitters, magnesium directly influences the hormones that govern the sleep-wake cycle. It plays a role in the regulation of melatonin, the body's primary sleep hormone, and helps to normalize the activity of the hypothalamic-pituitary-adrenal (HPA) axis, the body's central stress response system.19 Studies have shown that magnesium supplementation can lead to lower nocturnal levels of the stress hormone cortisol, creating a physiological environment more conducive to deep, restorative sleep.26
In the case of magnesium glycinate, these effects are further amplified by the glycine component. Glycine itself has been shown to have calming properties and can facilitate sleep onset, in part by helping to lower core body temperature, a natural signal for the body to prepare for sleep.19
Clinical Evidence
The clinical evidence supporting magnesium for sleep improvement is promising and growing. While many early studies were small or observational, more recent, high-quality research has provided stronger support. A landmark double-blind, placebo-controlled clinical trial conducted in elderly individuals with primary insomnia found that supplementation with 500 mg of magnesium for 8 weeks resulted in significant improvements across multiple sleep metrics. Participants in the magnesium group experienced longer sleep times, higher sleep efficiency, reduced sleep onset latency (the time it takes to fall asleep), and fewer instances of early morning awakening compared to the placebo group. These subjective improvements were corroborated by objective biochemical changes, including increased serum melatonin and renin levels and a significant decrease in serum cortisol.26
Building on this, a highly rigorous randomized, double-blind, placebo-controlled crossover trial published in 2024 provided compelling objective evidence. Using Oura Rings to track sleep patterns, the study found that magnesium supplementation (using magnesium chloride) led to statistically significant improvements in deep sleep, total sleep duration, and sleep efficiency when compared to placebo.30 Participants in the magnesium condition also reported better subjective sleep quality and mood. The use of objective wearable technology in this study adds significant weight to the claim that magnesium can tangibly improve sleep architecture.
While these robust trials used other forms of magnesium, the underlying mechanisms are related to restoring magnesium levels and modulating CNS activity—roles for which the highly bioavailable and neurologically active magnesium glycinate is an excellent candidate. Further research specifically comparing magnesium glycinate to other forms for sleep is warranted to confirm its theoretically superior efficacy.
Anxiety and Stress Management
Magnesium's anxiolytic (anxiety-reducing) properties are deeply intertwined with its role in regulating the body's stress response. The relationship between magnesium and stress is often described as a "vicious circle."
Mechanisms
The vicious circle concept posits that psychological or physical stress leads to an increase in stress hormones, which in turn causes the body to excrete more magnesium through the urine. This can deplete magnesium stores, causing a deficiency. A state of magnesium deficiency, in turn, enhances the body's susceptibility to stress by increasing neuronal excitability and HPA axis activity. This creates a self-perpetuating cycle where stress depletes magnesium, and low magnesium amplifies the stress response.31
Magnesium helps to break this cycle by acting at several key points in the stress pathway. It directly modulates the HPA axis, helping to attenuate the release of adrenocorticotropic hormone (ACTH) from the pituitary gland and thereby blunting the production of cortisol from the adrenal glands.9 By helping to regulate cortisol levels, magnesium prevents the over-activation of the body's stress response.27
At the neurotransmitter level, magnesium helps maintain a healthy balance between excitation and inhibition in the brain. It dampens the effects of the primary excitatory neurotransmitter, glutamate, by blocking its NMDA receptor, and it promotes the calming effects of the primary inhibitory neurotransmitter, GABA.27 This dual action helps to prevent the state of hyper-arousal and neuronal over-firing that underlies feelings of anxiety. Once again, the glycine in magnesium glycinate contributes directly to this calming effect through its own inhibitory actions in the CNS.22
Clinical Evidence
While the biological rationale for using magnesium to manage anxiety and stress is exceptionally strong, the clinical evidence from human trials is currently more suggestive than definitive. A comprehensive systematic review published in 2017 by Boyle et al. examined the existing evidence for magnesium supplementation on subjective anxiety.9 The review concluded that the evidence is
suggestive of a beneficial effect in anxiety-vulnerable populations (such as those with mild anxiety or premenstrual syndrome), but that the overall quality of the existing studies is poor.
The review highlighted significant methodological flaws in the research, including small sample sizes, a lack of appropriate placebo controls, failure to use validated measures of stress, and inconsistent statistical analysis.9 This means that while some individual studies have reported positive effects, the field as a whole lacks the high-quality, large-scale randomized controlled trials (RCTs) needed to make a firm conclusion. For example, one small 6-week study found that 248 mg of magnesium per day decreased symptoms of both depression and anxiety 2, but such studies are not sufficient to establish a standard of care.
This creates an "evidence-mechanism gap." The form of magnesium that is most compelling on a biochemical level for treating anxiety—magnesium glycinate, with its dual-action inhibitory mechanism—lacks specific, high-quality clinical trials to support its use. The evidence that does exist often uses other forms of magnesium and suffers from methodological weaknesses. Therefore, while magnesium glycinate represents a logical and safe choice for individuals seeking to support their nervous system and manage stress, it is important to acknowledge that its efficacy for clinical anxiety has not yet been rigorously proven to the standards of evidence-based medicine.
Migraine Prophylaxis and Treatment
In contrast to the state of anxiety research, the evidence supporting the use of magnesium in the management of migraine headaches is robust and has led to its inclusion in treatment guidelines.
Mechanisms
A link between low magnesium levels and migraine pathophysiology has been established for decades. It is understood that magnesium deficiency can lower the threshold for migraine attacks by influencing several key neurological and vascular pathways:
-
Inhibition of Cortical Spreading Depression (CSD): CSD is a slow-moving wave of intense neuronal and glial depolarization followed by a period of inactivity, which is believed to be the underlying cause of migraine aura and a trigger for headache pain. Magnesium helps to prevent CSD by stabilizing neuronal membranes and blocking NMDA receptors, which are critical for the propagation of the CSD wave.10
-
NMDA Receptor Antagonism: By blocking NMDA receptors, magnesium reduces central nervous system hyperexcitability and decreases the transmission of pain signals.34
-
Regulation of Vasoactive Peptides and Neurotransmitters: Magnesium helps to regulate the release and activity of several substances involved in migraine attacks. It can decrease levels of Calcitonin Gene-Related Peptide (CGRP), a potent vasodilator and pain-signaling molecule that is a major target of modern migraine drugs.10 It also modulates serotonin activity and nitric oxide production, both of which influence cerebral blood flow and vascular tone.10
Clinical Evidence
The clinical efficacy of magnesium for migraine has been demonstrated in numerous RCTs, systematic reviews, and meta-analyses. The evidence supports its use for both acute treatment and long-term prevention.
-
Migraine Prophylaxis (Prevention): Multiple studies have shown that daily oral magnesium supplementation can significantly reduce the frequency and intensity of migraine attacks. A 2016 meta-analysis of 10 RCTs concluded that oral magnesium was effective for both outcomes.34 One influential RCT found that a daily dose of 600 mg of trimagnesium dicitrate reduced migraine attack frequency by 41.6%, compared to just 15.8% in the placebo group.34 Based on such evidence, the American Headache Society and the American Academy of Neurology have issued guidelines suggesting that magnesium therapy is "possibly effective" for migraine prevention, with a typical recommended dose of 400-500 mg per day.34
-
Acute Migraine Treatment: For the treatment of an active migraine attack, intravenous (IV) magnesium sulfate has proven highly effective, particularly for patients experiencing aura. A meta-analysis of 11 studies found that a 1-gram infusion of IV magnesium significantly relieved acute migraine pain within 15-45 minutes of administration.34 Numerous individual RCTs corroborate this finding, showing rapid relief of headache, nausea, and photophobia compared to placebo or other standard treatments.10
While many of the clinical trials have used forms like magnesium citrate, oxide, or IV sulfate, the fundamental goal is to correct the magnesium deficiency that contributes to migraine susceptibility. For long-term prophylaxis, the highly bioavailable and well-tolerated magnesium glycinate represents an excellent choice, as it can effectively raise magnesium levels without the GI side effects that might limit adherence to other forms.
Clinical Applications and Evidence: Systemic and Musculoskeletal Health
Muscle Function, Pain, and Cramping
Magnesium is fundamentally linked to muscle physiology, playing a dual role in both contraction and, more critically, relaxation. This has led to its widespread use for muscle-related complaints, though the clinical evidence presents a complex picture.
Mechanisms
Magnesium's role in muscle relaxation is primarily mediated through its relationship with calcium. Muscle contraction is triggered by an influx of calcium ions into muscle cells. Magnesium acts as a natural physiological calcium channel blocker, competing with calcium for binding sites on the sarcoplasmic reticulum.2 By doing so, it helps to regulate calcium flow and prevent the state of sustained contraction that manifests as cramping or spasm. Furthermore, the process of pumping calcium back out of the muscle cell to allow it to relax is an active, energy-dependent process that requires ATP. As magnesium is essential for both the synthesis and function of ATP, a deficiency can impair this relaxation process, leading to excessive muscle tension, spasms, and tics.37
Clinical Evidence
Despite a strong mechanistic rationale and widespread popular belief, the clinical evidence for magnesium supplementation as a general remedy for muscle cramps is surprisingly weak. A landmark Cochrane Systematic Review, which represents one of the highest standards of evidence in medicine, analyzed the available data and concluded that it is unlikely that magnesium supplementation is effective for treating idiopathic skeletal muscle cramps (cramps with no known cause), particularly in older adults.5 The review also found that the evidence for pregnancy-associated cramps was conflicting and that the data for exercise-related cramps was unreliable.5
This creates a significant disconnect between the biochemical theory and the clinical trial results for common muscle cramps. This suggests that magnesium's benefits may not be universal but are instead confined to specific situations or populations. For example, cramps that are a direct result of a confirmed magnesium deficiency are likely to respond to supplementation. Similarly, its smooth muscle relaxation properties are being explored in more specific contexts, such as a clinical trial investigating intravenous magnesium for uterine cramping following gynecological procedures.39 For general exercise performance and muscle recovery, studies show some potential benefits for older adults or those with a known deficiency, but the results are mixed and do not support widespread use in active individuals with adequate magnesium levels.2 Therefore, caution should be exercised against overstating the benefits of magnesium for common muscle cramps, as its true value may be limited to conditions where deficiency or specific pathological pathways are the primary drivers.
Fibromyalgia and Chronic Fatigue Syndrome (CFS)
For complex, multi-system illnesses like fibromyalgia (FM) and chronic fatigue syndrome (ME/CFS), magnesium is of particular interest because its mechanisms of action align with several key aspects of their pathophysiology.
Mechanisms
The link between magnesium and these conditions is multifaceted. Both FM and ME/CFS are associated with disturbances in cellular energy metabolism, and low levels of ATP have been observed in the muscles of fibromyalgia patients.11 Given magnesium's indispensable role in ATP synthesis and the Krebs cycle, correcting a deficiency could theoretically improve cellular bioenergetics.
Perhaps more importantly, a core feature of fibromyalgia is central sensitization, a state of nervous system hypersensitivity mediated by the over-activation of NMDA receptors. Magnesium's function as a natural NMDA receptor antagonist is therefore highly relevant, as it could help to dampen this hypersensitivity and reduce pain perception.11 Additionally, magnesium deficiency can promote the release of Substance P, a pro-inflammatory neuropeptide involved in pain signaling that is known to be upregulated in fibromyalgia.11
Clinical Evidence
The clinical evidence for magnesium in these conditions is still considered preliminary but is generally promising.
-
Fibromyalgia: Several small trials suggest a benefit. A 2022 randomized, double-blind, placebo-controlled trial found that 100 mg of oral magnesium (as chloride) for one month significantly reduced pain severity in fibromyalgia patients. It also reduced stress levels, but only in the subgroup of patients with mild-to-moderate baseline stress.40 Other studies using magnesium citrate, either alone or in combination with the medication amitriptyline, have shown reductions in tender point counts and improvements in quality of life.37 Trials with magnesium malate have also reported some positive outcomes.38 While there are no major trials specifically on magnesium glycinate for fibromyalgia, its high bioavailability and GI tolerance make it a logical choice for delivering magnesium to target these mechanisms.
-
Chronic Fatigue Syndrome (ME/CFS): The evidence here is older and more limited. A key 1991 study by Cox et al. was influential, finding that a group of CFS patients had lower red blood cell magnesium levels compared to healthy controls. In a subsequent double-blind trial, they found that weekly intramuscular injections of magnesium sulfate for six weeks led to significant improvements in energy levels, emotional state, and pain compared to placebo.12 However, this finding has not been consistently replicated, with some subsequent smaller studies failing to find evidence of magnesium deficiency in their CFS cohorts.42
For both conditions, magnesium supplementation, particularly with a highly bioavailable form like glycinate, represents a plausible and safe adjunctive therapy that targets several potential underlying mechanisms. However, it is not considered a primary treatment, and larger, more rigorous clinical trials are needed to clarify its role and efficacy.
Cardiovascular and Metabolic Health
Magnesium plays a supportive role in cardiovascular and metabolic health, primarily through its influence on blood pressure and glucose metabolism.
Mechanisms
-
Blood Pressure: Magnesium helps to regulate vascular tone by promoting the relaxation of smooth muscle cells in blood vessel walls, leading to vasodilation (widening of blood vessels) and potentially lower blood pressure.3 It may also influence the renin-angiotensin-aldosterone system, a key hormonal cascade that controls blood pressure.43
-
Diabetes and Insulin Sensitivity: Magnesium is a crucial cofactor for the enzymes involved in glucose metabolism and insulin signaling. A deficiency can impair the body's ability to use insulin effectively, leading to insulin resistance, a hallmark of type 2 diabetes. Conversely, the high blood sugar levels characteristic of diabetes can increase the amount of magnesium lost in the urine, exacerbating the deficiency.3
Clinical Evidence
-
Hypertension: While mechanistically plausible, the effect of magnesium supplementation on blood pressure appears to be modest. A 2018 review noted its important role in heart health 3, but the Office of Dietary Supplements (ODS) concludes that, based on current research, magnesium supplements lower blood pressure "to only a small extent".3 Research is ongoing, including a registered RCT specifically testing the effect of 480 mg/day of magnesium glycinate on blood pressure in adults with untreated hypertension.43
-
Type 2 Diabetes: The evidence here is stronger, particularly for individuals with an existing deficiency. High dietary intake of magnesium is consistently linked with a lower risk of developing type 2 diabetes.3 A 2017 systematic review concluded that magnesium supplements can improve insulin sensitivity in people with low magnesium levels.3 An RCT using oral magnesium chloride demonstrated significant improvements in both insulin sensitivity and overall metabolic control in subjects with type 2 diabetes and low serum magnesium.14
In summary, magnesium serves as an important supportive nutrient for cardiovascular and metabolic health, especially for correcting deficiencies that can contribute to these conditions. It is not a standalone treatment for hypertension or diabetes, but ensuring adequate intake is a key part of a comprehensive management plan. Magnesium glycinate, with its high bioavailability and excellent safety profile for long-term use, is a suitable form for supplementation in these populations.
Practical Guidance: Dosage, Safety, and Drug Interactions
Dosing Recommendations: From RDA to Therapeutic Application
Effective and safe use of magnesium supplements requires an understanding of both standard dietary recommendations and the therapeutic doses used in clinical research. The Food and Nutrition Board at the Institute of Medicine has established a Recommended Dietary Allowance (RDA) for magnesium, which represents the average daily intake sufficient to meet the nutrient requirements of nearly all healthy individuals.
|
Table 2: Recommended Dietary Allowance (RDA) and Tolerable Upper Intake Level (UL) for Magnesium |
|||
|
Life Stage/Age Group |
Sex |
RDA (mg/day) |
UL for Supplements (mg/day) |
|
Children 1–3 years |
Male/Female |
80 mg |
65 mg |
|
Children 4–8 years |
Male/Female |
130 mg |
110 mg |
|
Children 9–13 years |
Male/Female |
240 mg |
350 mg |
|
Teens 14–18 years |
Male |
410 mg |
350 mg |
|
Teens 14–18 years |
Female |
360 mg |
350 mg |
|
Adults 19+ years |
Male |
400–420 mg |
350 mg |
|
Adults 19+ years |
Female |
310–320 mg |
350 mg |
|
Pregnancy |
14-18 years |
400 mg |
350 mg |
|
Pregnancy |
19+ years |
350–360 mg |
350 mg |
|
Lactation |
14-18 years |
360 mg |
350 mg |
|
Lactation |
19+ years |
310–320 mg |
350 mg |
Source: Office of Dietary Supplements, National Institutes of Health 46
It is crucial to note that the Tolerable Upper Intake Level (UL) of 350 mg/day for adults applies only to magnesium from dietary supplements and medications. It does not include magnesium naturally present in food and beverages, which is not considered harmful as the kidneys can excrete any excess in healthy individuals.46
Therapeutic dosages used in clinical trials to achieve specific health outcomes often exceed the UL. For instance, studies on migraine prevention have successfully used doses of 400-600 mg of elemental magnesium per day.34 An ongoing trial for blood pressure is using 480 mg/day of magnesium glycinate.43 Such doses should only be taken under the guidance of a healthcare professional who can assess the potential benefits against any risks.
When selecting a supplement, it is also important to understand the concept of elemental magnesium. The total weight of a capsule (e.g., 500 mg of magnesium glycinate) is not the same as the amount of actual magnesium it provides. Magnesium glycinate, for example, is approximately 14% elemental magnesium by weight.11 Therefore, a 500 mg capsule of magnesium glycinate provides about 70 mg of elemental magnesium. This distinction is vital for accurate dosing.
Safety Profile: Side Effects, Contraindications, and Toxicity
Magnesium supplements are generally considered safe for most people when taken at appropriate doses. However, there are potential side effects, contraindications, and risks of toxicity to consider.
-
Common Side Effects: The most frequent side effects are gastrointestinal and dose-dependent. These can include diarrhea, nausea, and abdominal cramping.7 These effects are most common with less bioavailable forms like magnesium oxide, which have a strong osmotic effect. Magnesium glycinate is widely recognized for being exceptionally gentle on the digestive system, minimizing these side effects even at higher doses.13
-
Contraindications: The primary contraindication for magnesium supplementation is renal impairment or kidney failure. Healthy kidneys are efficient at excreting excess magnesium, but when renal function is compromised, magnesium can accumulate in the body to toxic levels.4 Individuals with kidney disease should not take magnesium supplements unless directed and closely monitored by a physician. Caution is also advised for patients with certain neuromuscular diseases like myasthenia gravis, as magnesium can inhibit the release of acetylcholine at the neuromuscular junction and potentially worsen muscle weakness.6
-
Toxicity (Hypermagnesemia): Magnesium toxicity is rare in individuals with normal kidney function but can be life-threatening. It typically occurs from a massive overdose of magnesium-containing laxatives or antacids, or in patients with renal failure.6 Symptoms of hypermagnesemia progress as blood levels rise and include flushing, hypotension (low blood pressure), and hyporeflexia (impaired reflexes), which can advance to more severe effects like respiratory depression, cardiovascular collapse, and cardiac arrest at very high levels.6
Clinically Significant Drug Interactions
Magnesium supplements can interact with several common medications, either by affecting the drug's absorption or by having its own levels affected by the drug. It is essential to be aware of these interactions to prevent treatment failure or adverse effects.
|
Table 3: Clinically Significant Drug Interactions with Magnesium Supplements |
|||
|
Interacting Drug Class/Medication |
Example Drugs |
Mechanism of Interaction |
Clinical Management/Recommendation |
|
Bisphosphonates |
Alendronate (Fosamax), Ibandronate (Boniva) |
Magnesium forms insoluble chelates with bisphosphonates, significantly reducing their absorption and efficacy in treating osteoporosis. 8 |
Separate doses. Take the bisphosphonate at least 2 hours before or after taking any magnesium-containing product. 47 |
|
Tetracycline Antibiotics |
Doxycycline, Minocycline, Tetracycline |
Magnesium binds to tetracyclines in the gut, forming complexes that are poorly absorbed. This can lead to lower antibiotic levels and potential treatment failure. 8 |
Separate doses. Take the antibiotic at least 2 hours before or 4-6 hours after the magnesium supplement. 47 |
|
Fluoroquinolone Antibiotics |
Ciprofloxacin (Cipro), Levofloxacin |
Similar to tetracyclines, magnesium chelates with fluoroquinolones, impairing their absorption and reducing their effectiveness. 8 |
Separate doses. Take the antibiotic at least 2 hours before or 4-6 hours after the magnesium supplement. 47 |
|
Diuretics (Loop and Thiazide) |
Furosemide (Lasix), Hydrochlorothiazide (HCTZ) |
These types of diuretics increase the renal excretion (loss) of magnesium in the urine, which can lead to magnesium deficiency over time. 8 |
A healthcare provider may need to monitor magnesium levels in patients on long-term diuretic therapy and recommend supplementation if necessary. |
|
Proton Pump Inhibitors (PPIs) |
Omeprazole (Prilosec), Esomeprazole (Nexium) |
Long-term use of PPIs (typically >1 year) has been shown to impair intestinal absorption of magnesium, leading to hypomagnesemia. 1 |
Patients on long-term PPI therapy should have their magnesium levels monitored periodically. Supplementation may be required. |
|
Gabapentin |
Neurontin |
Magnesium can decrease the absorption of gabapentin by up to 20-40%, potentially reducing its effectiveness for seizures or nerve pain. 47 |
Separate doses. Take gabapentin at least 2 hours after taking a magnesium supplement. 47 |
Synthesis and Recommendations
Summary of Evidence by Clinical Indication
The clinical and mechanistic review of magnesium, and specifically magnesium glycinate, reveals a varied landscape of evidence. The strength of the recommendation for its use depends heavily on the specific health condition being addressed.
-
Strong Evidence:
-
Migraine Prophylaxis: A robust body of evidence from multiple meta-analyses and RCTs supports the use of daily oral magnesium to reduce the frequency and intensity of migraine attacks. It is included in professional treatment guidelines.
-
Moderate/Promising Evidence:
-
Sleep Quality: Recent high-quality trials, including one with objective wearable data, provide compelling evidence that magnesium can improve multiple aspects of sleep, including sleep duration and deep sleep, particularly in those with poor sleep.
-
Fibromyalgia and Chronic Fatigue Syndrome: Preliminary evidence suggests magnesium may serve as a beneficial adjunctive therapy by targeting key pathophysiological mechanisms like central sensitization and energy metabolism, but larger trials are needed.
-
Type 2 Diabetes: Strong evidence indicates that magnesium supplementation can improve insulin sensitivity and glycemic control in individuals with type 2 diabetes who are also magnesium deficient.
-
Suggestive but Weak/Poor Quality Evidence:
-
Anxiety and Stress: While the mechanistic rationale is exceptionally strong, the existing human clinical trial evidence is deemed to be of poor quality, preventing a definitive recommendation. Magnesium's role is plausible but not yet rigorously proven.
-
Conflicting/Negative Evidence:
-
Idiopathic Muscle Cramps: Despite its popularity for this use, the highest level of evidence from a Cochrane Review concludes that magnesium is unlikely to be effective for common muscle cramps in the general adult population.
Considerations for Clinical Practice and Personal Use
Based on the available evidence, magnesium glycinate emerges as a premier choice among magnesium supplements for several reasons. Its high bioavailability ensures efficient absorption, while its superior gastrointestinal tolerance makes it suitable for long-term use, for individuals with sensitive digestive systems, and when higher therapeutic doses are required. Its dual-action nature, delivering both magnesium and the inhibitory neurotransmitter glycine, makes it a theoretically ideal candidate for neurological and psychological applications like sleep and stress management.
For personal use, it is generally advisable to start with a lower dose (e.g., 100-200 mg of elemental magnesium per day) and gradually titrate upwards as needed to assess individual tolerance and response. It is paramount to consult with a qualified healthcare provider before beginning any new supplement regimen. This is especially critical for individuals with pre-existing medical conditions (particularly kidney disease), those who are pregnant or breastfeeding, and anyone taking medications that may interact with magnesium. A healthcare provider can help determine the appropriateness of supplementation, recommend a suitable dose, and monitor for any potential adverse effects.
Future Research Directions
While the understanding of magnesium's role in health has advanced significantly, several key areas require further investigation to solidify its place in clinical practice.
-
There is a clear need for large-scale, high-quality randomized controlled trials focused specifically on magnesium glycinate to validate its efficacy for anxiety, stress, and sleep disorders. Such trials would help bridge the current gap between its strong mechanistic rationale and the limited clinical evidence.
-
Comparative effectiveness trials that directly compare different forms of magnesium (e.g., glycinate vs. citrate vs. L-threonate) for specific neurological outcomes would be invaluable for guiding clinical recommendations.
-
Future studies should incorporate more accurate measures of baseline magnesium status, such as red blood cell magnesium, rather than relying solely on serum levels. This would allow researchers to better identify deficient populations and determine if baseline status predicts treatment response.
-
Further research into optimal dosing strategies and the long-term safety and efficacy of therapeutic doses exceeding the current UL is warranted for conditions like migraine and fibromyalgia.
Works cited
-
Magnesium in Man: Implications for Health and Disease | Physiological Reviews, accessed June 26, 2025, https://journals.physiology.org/doi/abs/10.1152/physrev.00012.2014
-
What Are the Health Benefits of Magnesium? - Healthline, accessed June 26, 2025, https://www.healthline.com/nutrition/magnesium-benefits
-
Magnesium: Health benefits, deficiency, sources, and risks, accessed June 26, 2025, https://www.medicalnewstoday.com/articles/286839
-
Magnesium in diet: MedlinePlus Medical Encyclopedia, accessed June 26, 2025, https://medlineplus.gov/ency/article/002423.htm
-
What is the role of magnesium for skeletal muscle cramps? A ..., accessed June 26, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC8020016/
-
Magnesium - StatPearls - NCBI Bookshelf, accessed June 26, 2025, https://www.ncbi.nlm.nih.gov/books/NBK519036/
-
Magnesium Supplements: Benefits, Deficiency, Dosage, Effects, and More - WebMD, accessed June 26, 2025, https://www.webmd.com/diet/supplement-guide-magnesium
-
5 Medications To Not Mix With Magnesium - Health, accessed June 26, 2025, https://www.health.com/medications-not-to-mix-with-magnesium-8687830
-
The Effects of Magnesium Supplementation on Subjective Anxiety and Stress—A Systematic Review - PMC - PubMed Central, accessed June 26, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC5452159/
-
Magnesium and Migraine - MDPI, accessed June 26, 2025, https://www.mdpi.com/2072-6643/17/4/725
-
Mitochondrial Enhancers for ME/CFS and Fibromyalgia Pt III ..., accessed June 26, 2025, https://www.healthrising.org/blog/2021/08/06/mitochondria-chronic-fatigue-syndrome-fibromyalgia-magnesium/
-
Red blood cell magnesium and chronic fatigue syndrome - PubMed, accessed June 26, 2025, https://pubmed.ncbi.nlm.nih.gov/1672392/
-
Magnesium Citrate vs. Glycinate: Which is Better? | Nature Made®, accessed June 26, 2025, https://www.naturemade.com/blogs/health-articles/magnesium-citrate-vs-glycinate
-
Types Of Magnesium Supplements - Consensus Academic Search Engine, accessed June 26, 2025, https://consensus.app/questions/types-of-magnesium-supplements/
-
Everything You Should Know About Magnesium Glycinate ..., accessed June 26, 2025, https://consensus.app/home/blog/everything-you-should-know-about-magnesium-glycinate/
-
8 Types of Magnesium and Their Benefits - Verywell Health, accessed June 26, 2025, https://www.verywellhealth.com/types-of-magnesium-what-they-are-and-how-to-choose-8748803
-
Different Types of Magnesium: Which One Should You Take? - Health, accessed June 26, 2025, https://www.health.com/types-of-magnesium-7853312
-
What Are the Different Types of Magnesium?, accessed June 26, 2025, https://www.blazma.com/blogs/137?lang=en
-
How Magnesium Glycinate Promotes Restful Sleep - Nava Health, accessed June 26, 2025, https://navacenter.com/how-magnesium-glycinate-can-be-your-key-to-restful-sleep/
-
Magnesium glycinate: Benefits, side effects, dosage, and more - Medical News Today, accessed June 26, 2025, https://www.medicalnewstoday.com/articles/315372
-
Magnesium Glycinate - Unived, accessed June 26, 2025, https://unived.com/blogs/articles/magnesium-glycinate-a-highly-absorbable-form
-
www.acnp.org, accessed June 26, 2025, https://www.acnp.org/g4/GN401000008/Default.htm#:~:text=Glycine%20is%20the%20major%20inhibitory,of%20motor%20and%20sensory%20functions.
-
GABA and Glycine - ACNP, accessed June 26, 2025, https://www.acnp.org/g4/GN401000008/Default.htm
-
Glycine Receptors - Basic Neurochemistry - NCBI Bookshelf, accessed June 26, 2025, https://www.ncbi.nlm.nih.gov/books/NBK28003/
-
Neurotransmitters: What They Are, Functions & Types - Cleveland Clinic, accessed June 26, 2025, https://my.clevelandclinic.org/health/articles/22513-neurotransmitters
-
Does Magnesium Glycinate Really Help You Sleep Better? - Consensus, accessed June 26, 2025, https://consensus.app/home/blog/does-magnesium-glycinate-really-help-you-sleep-better/
-
Magnesium for Anxiety: Does It Help? - Cleveland Clinic Health Essentials, accessed June 26, 2025, https://health.clevelandclinic.org/magnesium-for-anxiety
-
Does Magnesium for Anxiety Really Work? - Verywell Health, accessed June 26, 2025, https://www.verywellhealth.com/magnesium-for-anxiety-8412089
-
Magnesium Glycinate: The Natural Solution for Anxiety, Chronic Stress - Sois Life Sciences, accessed June 26, 2025, https://www.soislifesciences.com/blogs/wellness-blogs/magnesium-glycinate-the-natural-solution-for-anxiety-chronic-stress-and-better-sleep
-
(PDF) Effectiveness of Magnesium Supplementation on Sleep ..., accessed June 26, 2025, https://www.researchgate.net/publication/378318255_Effectiveness_of_Magnesium_Supplementation_on_Sleep_Quality_and_Related_Health_Outcomes_for_Adults_with_Poor_Sleep_Quality_A_Randomized_Double-Blind_Placebo-Controlled_Crossover_Trial
-
Magnesium Status and Stress: The Vicious Circle Concept Revisited ..., accessed June 26, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC7761127/
-
Effect of a Dietary Supplement Combining Bioactive Peptides and Magnesium on Adjustment Disorder with Anxiety: A Clinical Trial in General Practice - MDPI, accessed June 26, 2025, https://www.mdpi.com/2072-6643/14/12/2425
-
The Effects of Magnesium Supplementation on Subjective Anxiety and Stress-A Systematic Review - PubMed, accessed June 26, 2025, https://pubmed.ncbi.nlm.nih.gov/28445426/
-
Does magnesium help with headaches and migraines? - Drugs.com, accessed June 26, 2025, https://www.drugs.com/medical-answers/magnesium-help-headaches-migraines-3579523/
-
Effects of Intravenous and Oral Magnesium on Reducing Migraine: A Meta-analysis of Randomized Controlled Trials - :::::Pain Physician:::::, accessed June 26, 2025, https://www.painphysicianjournal.com/current/pdf?article=MjQ4Nw==&journal=93
-
Magnesium in Migraine Prophylaxis-Is There an Evidence-Based Rationale? A Systematic Review | Request PDF - ResearchGate, accessed June 26, 2025, https://www.researchgate.net/publication/321037519_Magnesium_in_Migraine_Prophylaxis-Is_There_an_Evidence-Based_Rationale_A_Systematic_Review
-
Magnesium Supplements: What's Their Role In Fibromyalgia ..., accessed June 26, 2025, https://www.synergyrheum.com/magnesium-supplements-role-in-fibromyalgia/
-
Magnesium in the Treatment of Fibromyalgia - Relias Media, accessed June 26, 2025, https://www.reliasmedia.com/articles/116358-magnesium-in-the-treatment-of-fibromyalgia
-
Study Details | Magnesium and Cramping | ClinicalTrials.gov, accessed June 26, 2025, https://www.clinicaltrials.gov/study/NCT06745388?cond=%22Muscle%20Cramp%22&viewType=Table&rank=9
-
(PDF) Short-Term Magnesium Therapy Alleviates Moderate Stress in Patients with Fibromyalgia: A Randomized Double-Blind Clinical Trial - ResearchGate, accessed June 26, 2025, https://www.researchgate.net/publication/360656092_Short-Term_Magnesium_Therapy_Alleviates_Moderate_Stress_in_Patients_with_Fibromyalgia_A_Randomized_Double-Blind_Clinical_Trial
-
Short-Term Magnesium Therapy Alleviates Moderate Stress in Patients with Fibromyalgia: A Randomized Double-Blind Clinical Trial - PubMed Central, accessed June 26, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC9145501/
-
Magnesium - MEpedia, accessed June 26, 2025, https://me-pedia.org/wiki/Magnesium
-
Record History | ver. 7: 2022-08-03 | NCT03688503 | ClinicalTrials.gov, accessed June 26, 2025, https://www.clinicaltrials.gov/study/NCT03688503?tab=history&a=7
-
Magnesium Supplements: Benefits and Side Effects - Healthline, accessed June 26, 2025, https://www.healthline.com/nutrition/magnesium-supplements
-
Study Details | Magnesium Supplementation and Blood Pressure Reduction | ClinicalTrials.gov, accessed June 26, 2025, https://clinicaltrials.gov/study/NCT03688503
-
Magnesium - Consumer - NIH Office of Dietary Supplements, accessed June 26, 2025, https://ods.od.nih.gov/factsheets/Magnesium-Consumer/
-
8 Magnesium Interactions You Should Know About - GoodRx, accessed June 26, 2025, https://www.goodrx.com/well-being/supplements-herbs/magnesium-interactions
-
www.goodrx.com, accessed June 26, 2025, https://www.goodrx.com/well-being/supplements-herbs/magnesium-interactions#:~:text=Magnesium%20can%20lower%20the%20absorption%20of%20certain%20antibiotics%20and%20antiviral,magnesium%20levels%20in%20the%20body.